Weaning Your Baby
Weaning is the term most commonly used to describe the introduction of solid foods to your baby’s diet. However, this broader term actually includes the introduction of non-milk drinks or infant formula, as the reliance on breast milk ceases. Infancy is the most rapid period of growth in all areas of development. Generally, babies grow around 150-200g per week in the first four months of life, and 100-150g per week up until the 6-month mark. Continued good nutrition as your baby grows is paramount to protecting them against stunted growth, obesity and development of chronic diseases in adulthood. It also improves cognitive development and future bone mass.
All breastfed babies are eventually weaned, and when it occurs is strictly up to the mother and baby’s circumstances. For the first 6 months of life, breastmilk provides all the nourishment your baby needs. From 6 months onwards, the weaning process will begin once your baby starts to consume anything other than breastmilk, including solid foods, water juice and other milks.
Baby-Led vs Mother-Led Weaning
Weaning can be baby-led or mother-led. Sometimes, your baby will decide when they have had enough breast milk, or will refuse to be fed from the breast. This can be disappointing for the mother, but it is a perfectly natural process. Similarly, the mother can decide when she has had enough and wishes to cease breastfeeding. This can be due to a number of factors. Your baby may like frequent feeds during the night, which can be difficult to sustain. You may have been advised against breastfeeding for medical reasons, or if you wish to become pregnant again, breastfeeding may interfere with ovulation. Generally, a good way to encourage weaning is the “don’t offer, don’t refuse” method. You can stop offering the breast voluntarily, but don’t refuse it if your baby asks.
How to Wean
Gradual weaning is the best situation for your baby, as it gives them time to adjust. It also allows your milk supply to slowly decrease. Ways to plan the weaning process include:
- Weaning them onto a cup or bottle
- Start skipping the breastfeed that your baby is least interested in, and then cut back to ne every few days, week etc.
- Depending on age and other foods being introduced, you can replace the missed feeds with CREATIVE infant formula, cow’s milk or water. If your baby is under 12 months old, any missed breast feeds will need to be replaced with formula.
- Express some milk if your breasts become engorged
- Give your baby a dummy for extra sucking if they need it
- If possible, feed your baby to a fixed routine
Bottle Feeding
Generally, it is advised not to use bottles for feeding in the first 4 weeks of life as this can interfere with the natural processes of breastfeeding, which should be established first and foremost. During the weaning process however, you will eventually find you need to replace your breasts with bottles. Drop one nursing every few days initially and substitute with a bottle, so your baby and milk levels have time to adjust.

Good bottle-feeding practice includes:
- Checking the temperature of the milk or formula before feeding by squeezing a little of the contents out onto their wrist
- Cuddling and keeping contact with your baby while feeding
- Not leaving the infant to feed on their own
- Not putting your infant to sleep while drinking from a bottle. This can increase the risk of choking and dental issues
Introducing Solids
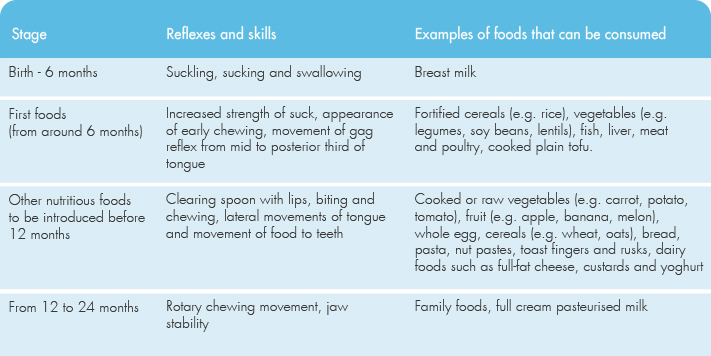
From around 6 months of age onwards, your infant will be able to adapt to different types of foods and feeding methods. Introduction of solid foods at this time is necessary to meet the infant’s increasing nutritional needs. Signs that that they’re ready for solid foods include:
- Sitting without support, increasing the ability to chew and swallow
- Tongue extrusion reflex (tongue thrust) subsides, allowing for acceptance of spoons and non-liquid foods
- Reaching for objects and bringing them to the mouth
- Bringing food to the mouth, chewing, then reaching for more
- Feeding behaviour progressing from sucking to biting (most infants are chewing by 7-9 months)
- Appetite is no longer satisfied by breastfeeding alone, indicating further nutritional needs
Stores of several nutrients including iron and zinc are often depleted in exclusively milk-fed infants, with iron levels being in particular need of supplementing after 6 months. Around this time, your baby’s digestive system will have matured in order to digest starches and as they become more interested in their environment, a willingness to try new flavours and textures will emerge.
What Foods to Introduce?
The introduction of solid foods at around 6 months should begin with iron-containing foods, including iron-enriched infant cereals, pureed meat, poultry and fish, or cooked tofu and legumes. As long as these iron-rich foods are added to the diet first, vegetables, fruits, and dairy products such as full-fat yoghurt, cheese and custard can then be added in any order. CREATIVE’s range of infant pureés are scientifically designed to meet all your growing baby’s nutritional needs during this period of rapid change.
- From 6 months, infants should be offered pureés and then mashed foods
- By 8 months most infants can manage ‘finger foods’
- By 12 months, infants can consume the same foods eaten by the rest of the family for a wider variety of nutritional choices